Cow’s Milk Allergy vs lactose intolerance: What is the difference?
Correct diagnosis of Cow’s Milk Allergy (CMA) and lactose intolerance (LI) helps ensure appropriate management and avoid unnecessary dietary restriction.1-3 Infants very rarely need a prolonged lactose-free or low-lactose diet.
Learn the key differences of CMA and LI below from our newest education piece reviewed and approved by Paediatric Gastroenterologist, Dr Rupert Hinds.

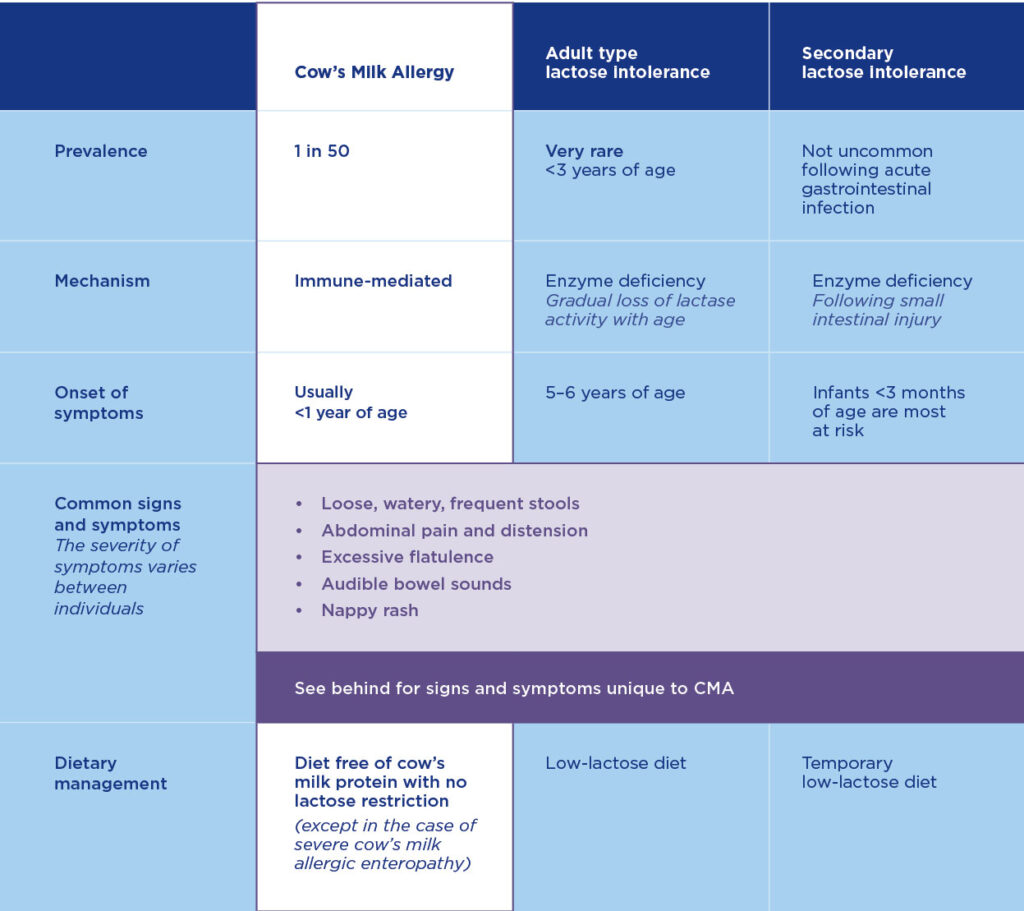
What is the difference between cow’s milk allergy and lactose intolerance?
Cow’s milk allergy (CMA) is caused by the immune system reacting to the protein found in cow’s milk and other dairy products. Lactose intolerance, however, is caused by a deficiency of the enzyme lactase.4,5 The possibility of a CMPA diagnosis should not be dismissed if an infant or child appears to be thriving and growing well.
What is the difference between cow’s milk allergy and cow’s milk intolerance?
Cow’s milk allergy has now replaced the term cow’s milk intolerance, which was previously used as a term for “non-IgE mediated CMA”.14 The term “allergy” acknowledges the involvement of the immune system.16 CMA babies can react to even the smallest amount of cow’s milk protein; therefore, the term CMI should no longer be used.
Signs and symptoms of lactose intolerance vs cow’s milk allergy
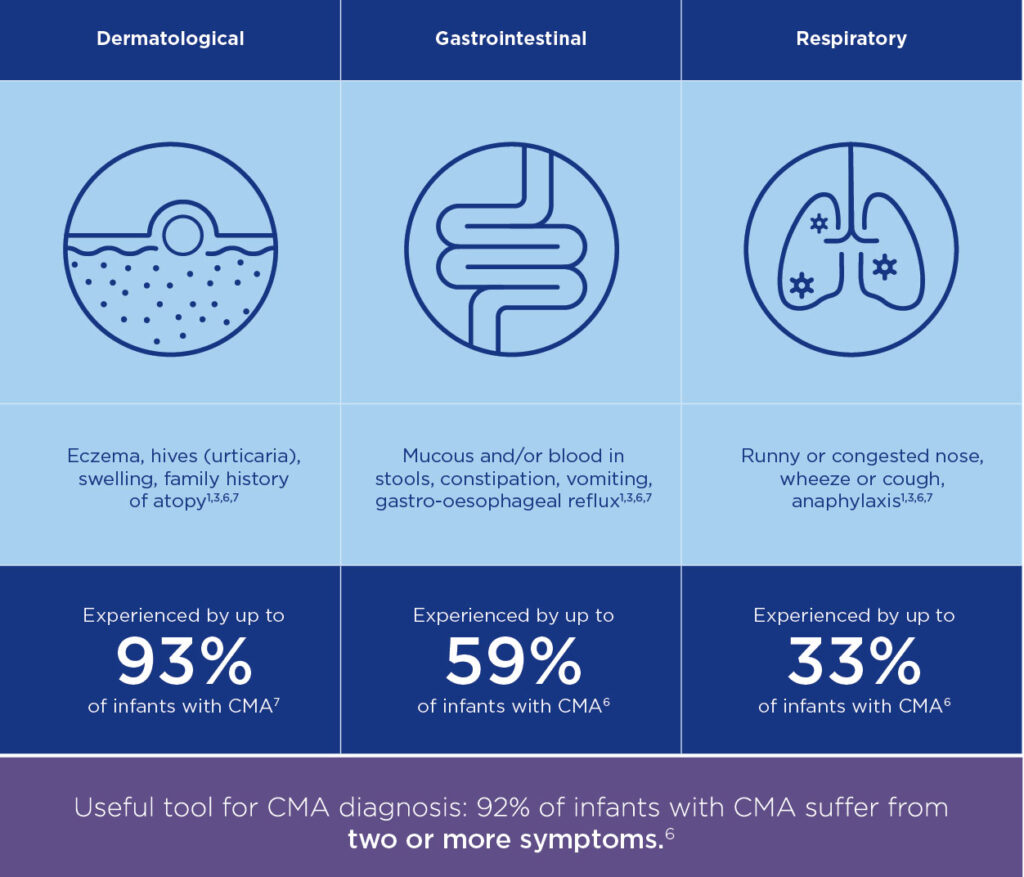
Lactose intolerance & cow’s milk allergy are often difficult to diagnose in babies and young children as they both present with similar gastrointestinal symptoms (GI). These may include symptoms such as nausea, vomiting, abdominal discomfort, bloating, diarrhoea, blood or mucus in the stool or allergic colitis. They may also display failure to thrive (FTT) in infancy. In most cases, these GI symptoms are caused by an allergic reaction to cow’s milk protein, rather than lactose intolerance.10
CMA infants and children may also have a family history of atopy and display skin and respiratory symptoms, such as acute urticaria and/or angioedema, atopic eczema, congestion, cough, wheezing, shortness of breath.1 Lactose intolerance does not display these types of symptoms, as it does not involve the immune system.5,6,15 CMA usually appears during infancy, while lactose intolerance usually starts after 4-5 years of age.6
How common is cow’s milk allergy and lactose intolerance in infants?
CMA is one of the most common allergies seen in infants in Australia and New Zealand, with a prevalence of more than 2% (1/50) and usually develops within the first year of life.2,5,15
Primary lactose intolerance does not usually manifest clinically before 5 years of age.2 Lactose intolerance in young infants is typically secondary lactose intolerance, which is transient to an infection. It usually improves with resolution of the underlying condition, or as the patient recovers from gastroenteritis.3
How to diagnose CMA and lactose intolerance?
The cornerstone of CMA diagnosis is an allergy-focused history which includes the key questions that need to be addressed when milk allergy is suspected. An IgE-mediated allergic reaction to cow’s milk can be obvious as symptoms are usually rapid and occur shortly after consuming the cow’s milk allergen. Non-IgE mediated CMA can be more challenging as symptoms are usually delayed and occur two or more hours after consuming the cow’s milk allergen.
To confirm CMA diagnosis, you should take a medical history and trial exclusion of all cow’s milk protein from the maternal diet (and infant diet if mixed feeding) for a period of 2-4 weeks. Followed by re-introduction of the milk allergen and recurrence of symptoms to confirm a CMA diagnosis.13 If it is still unclear after re-introduction, urgently refer the patient to a specialist for proper clinical diagnosis.
For diagnosing lactose intolerance in infancy, stool tests (for reducing substances) as well as breath hydrogen tests are not helpful.20 A clinical history of gastroenteritis or associated stool testing for infections may be useful. This is a guide only. You should not use this information to diagnose a health or medical condition or problem, or alter, commence, or delay any medical treatment.
Full version of CMA vs LI detailer
Download the full detailer on the key differences between Cow’s Milk Allergy (CMA) and lactose intolerance (LI).
Find out moreCow’s Milk Allergy vs lactose intolerance – Frequently asked questions
Should the breastfeeding mother remove cow’s milk and soy from her diet if CMA is suspected?
If CMA is suspected the breastfeeding mother should trial a 2–4-week cow’s milk only elimination diet and all ingredients derived from cow’s milk should be excluded.13 Up to 40% of children with non-IgE mediated CMA will also be allergic to soy protein18, therefore the mother may also be recommended to exclude soy from her diet and follow a similar elimination followed by reintroduction process, to confirm diagnoses.17 Dietetic support should be encouraged to enable the mother’s diet to be nutritionally adequate with minimal dietary restrictions.
What formulas are appropriate for CMA?
There are several different types of specialised formulas appropriate for managing cow’s milk allergy. Hypoallergenic formulas include evidence-based extensively hydrolysed formulas (EHF), amino acid-based formulas (AAF) and hydrolysed rice protein-based formulas (HRPF); these formulas are studied in cow’s milk allergic infants. Soy formula may be suitable for the management of infants from 6-months of age with cow’s milk allergy and without soy allergy.9,10 Always check ASCIA’s guide for cow’s milk substitutes when determining which formula is most appropriate for your patient. If a severe reaction or anaphylaxis is present, you suspect FPIES or enteropathy, you should discuss suitable formula choice with an allergist, paediatrician or gastroenterologist prior to recommending an alternative to your patient.
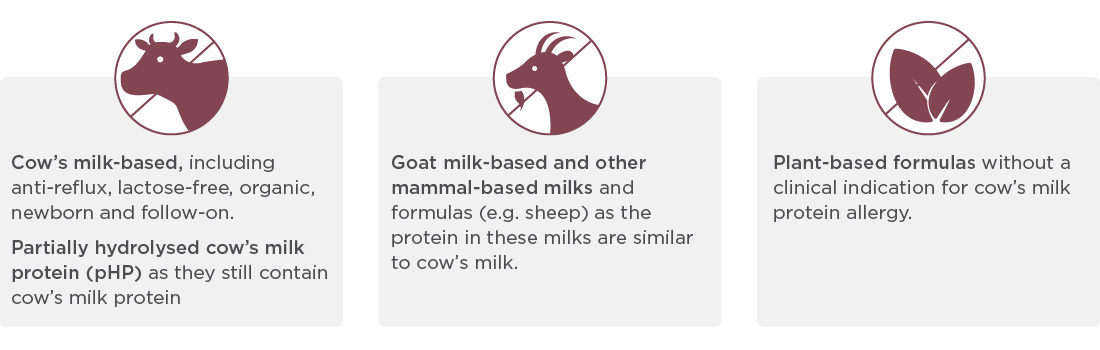
What formulas are NOT appropriate for CMA?
All formulas listed below are NOT suitable for an infant with a cow’s milk protein allergy.1 Parents and carers should always read the label carefully and choose a formula that is clinically indicated for cow’s milk protein allergy specifically.9
- Cow’s milk based
- Goat
Should breastfeeding mother’s trial a lactose free formula first, before trialling a hypoallergenic formula?
No, whether it is CMA or secondary transient lactose intolerance, following a GI condition such as gastroenteritis that is suspected, removing lactose from the breastfeeding mother’s diet will not improve symptoms. Lactose is the primary natural sugar present in breast milk.8 Whether the breastfeeding mother keeps or removes lactose in her diet, the amount of lactose in breastmilk is not related to the amount consumed through the diet.7
Should a breastfeeding mother remove lactose from her diet if her baby is experiencing symptoms?
No, primary lactose intolerance does not manifest clinically before 5 years of age.2 Lactose intolerance in young infants is typically secondary lactose intolerance caused by underlying gut conditions such as gastroenteritis, it is usually transient and improves with resolution of the underlying condition.3 Therefore, if the infant has not suffered any GI conditions recently, a cow’s milk elimination diet or hypoallergenic formula should be trialled immediately, not lactose free.
What support services are available for parents and carers of CMA and lactose intolerance infants?
There are several allergy support services available for parents and carers of CMA and lactose intolerance infants. These include:
Helpful tools for diagnosing CMA and LI
Treatment timelines and options may vary depending on your patient’s age and the severity of their symptoms. Understand more about your patient’s treatment pathway by using our helpful Diagnostic and Treatment Algorithms.
Diagnostic Algorithm
Two or more symptoms is a useful tool that can be used to diagnose CMPA.
Download nowTreatment Algorithm
A useful tool with the treatment pathway for diagnosed Cows’ Milk Protein Allergy.
Download nowOther useful resources
Related Products
Aptamil® AllerPro Syneo™ 1 (0-6 months)
Aptamil® AllerPro Syneo™ 2 (6-12 months)
Meet our Careline experts

References
- Di Costanzo MD and Canani RB. Ann Nutr Metab. 2018;73(Suppl 4):30–7.
- Heine RG, AlRefaee F, Bachina P, De Leon JC, Geng L, Gong S, Madrazo JA, Ngamphaiboon J, Ong C, Rogacion JM. Lactose intolerance and gastrointestinal cow’s milk allergy in infants and children – common misconceptions revisited. World Allergy Organ J. 2017 Dec 12;10(1):41. doi: 10.1186/s40413-017-0173-0. PMID: 29270244; PMCID: PMC5726035.
- Waddell L. What do we know about lactose? Complete Nutrition. 2016; 15(6):73-78.
- Crittenden RG, Bennett LE. Cow’s Milk Allergy: A Complex Disorder. J Am Coll Nutr. 2005;24(sup6):582S-591S.
- Fiocchi A, Brozek J, Schünemann H, Bahna SL, von Berg A, Beyer K, et al. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow’s Milk Allergy (DRACMA) Guidelines. World Allergy Organ J. 2010;3(4):57–161
- Walsh J et al. Br J Gen Pract 2016;66(649):e609–11.
- Maslin K, Fox A, Chambault M et al. Palatability of hypoallergenic formulas for cow’s milk allergy and healthcare professional recommendation. Pediatr Allergy Immunol. 2018;29:857–86
- Francavilla R, Calasso M, Calace L, Siragusa S, Ndagijimana M, Vernocchi P, Brunetti L, Mancino G, Tedeschi G, Guerzoni E, Indrio F, Laghi L, Miniello VL, Gobbetti M, De Angelis M. Effect of lactose on gut microbiota and metabolome of infants with cow’s milk allergy. Pediatr Allergy Immunol. 2012 Aug;23(5):420-7.
- ASCIA. Guide for Milk Substitutes in Cow’s Milk Allergy. 2022. (Cited 2022 April 7th). Available from: https://www.allergy.org.au/hp/papers/guide-for-milk-substitutes-cows-milk-allergy
- Kemp AS, Hill DJ, Allen KJ et al. Guidelines for the use of infant formulas to treat cow’s milk allergy: an Australian consensus panel opinion. Med J Aust. 2008 Jan 21;188(2):109–12.
- Bach AC, Babayan VK. Medium-chain triglycerides: an update. Am J Clin Nutr. 1982 Nov;36(5):950-62.
- Koletzko B, Lien E, Agostoni C, Böhles H, Campoy C, Cetin I, Decsi T, Dudenhausen JW, Dupont C, Forsyth S, Hoesli I, Holzgreve W, Lapillonne A, Putet G, Secher NJ, Symonds M, Szajewska H, Willatts P, Uauy R; World Association of Perinatal Medicine Dietary Guidelines Working Group. The roles of long-chain polyunsaturated fatty acids in pregnancy, lactation and infancy: review of current knowledge and consensus recommendations. J Perinat Med. 2008;36(1):5-14.
- Meyer R, Chebar Lozinsky A, Fleischer DM, Vieira MC, Du Toit G, Vandenplas Y, Dupont C, Knibb R, Uysal P, Cavkaytar O, Nowak-Wegrzyn A, Shah N, Venter C. Diagnosis and management of Non-IgE gastrointestinal allergies in breastfed infants-An EAACI Position Paper. Allergy. 2020 Jan;75(1):14-32.
- Ludman et al. Managing Cow’s Milk Allergy in Children. BMJ 2013; 347:5424
- Cow`s milk (dairy) allergy – Australasian Society of Clinical Immunology and Allergy (ASCIA), viewed December 2022 https://allergy.org.au/patients/food-allergy/cows-milk-dairy-allergy/
- Allergy or intolerance? – Food Intolerance Network (fedup.com.au), viewed January 2013 https://www.fedup.com.au/factsheets/support-factsheets/allergy-or-intolerance/
- ASCIA. Dietary Guide for Food Allergy Cow’s Milk Protein (Dairy) and Soy [internet]. Australia; 2021 [cited 2022 April 25]: https://www.allergy.org.au/ images/pcc/ASCIA_PCC_Dietary_avoidance_cows_milk_soy_July_2021.pdf/
- Cow’s milk allergy | Healthy Eating Advisory Service
https://heas.health.vic.gov.au/early-childhood-services/allergy-and-intolerance/cows-milk-allergy/ - Cow’s Milk Protein Allergy (CMPA); What to eat while breastfeeding when your baby has a cow’s milk protein allergy (infinitypediatrics.ca) http://infinitypediatrics.ca/wp-content/uploads/2015/01/Infinity-Pediatrics-CMPA-Breastfeeding.pdf/
- Heyman MB; Committee on Nutrition. Lactose intolerance in infants, children, and adolescents. Pediatrics. 2006 Sep;118(3):1279-86.
Support for you and your patients
Join now and learn about our education events, research initiatives and evidence-based resources – furthering your professional development and clinical practice.
Support for you and your patients
Support for you and your patients
Join now and learn about our education events, research initiatives and evidence-based resources – furthering your professional development and clinical practice.
