Infant Colic

Prevalence
After birth, 1 out of 2 children will develop what is collectively termed ‘functional gastrointestinal disorders’ – infantile colic is one of the most common problems affecting around 20% of infants up to 12 months of age.1
What is infantile colic?
Infantile colic remains quite misunderstood. All babies cry, and it is normal for crying patterns to increase week by week – peaking at around six to eight weeks of age.2 The general definition, based on the Rome IV criteria, is an infant who is under 5 months of age when symptoms peak, experiencing recurrent and prolonged periods of crying, fussing or irritability that occurs without cause and cannot be prevented or resolved by a carer, paired with no evidence of infant failure to thrive, fever or illness.3 Colic can have an adverse impact on an infant’s feeding habits, such as the premature cessation of breastfeeding.4 Left unresolved, infantile colic can have a negative impact on parents and babies from a family dynamic and financial perspective.5-8
What are the signs and symptoms?
The symptoms of infantile colic may include recurrent and prolonged periods of crying, fussing or irritability without an obvious cause.3 Other, more immediate signs include crying that:3
- Develops early and peaks at 6-8 weeks
- Worsens in the afternoon or evening
- Lasts several hours
- Improves at 3-4 months
Infantile colic treatment
For a family whose baby is experiencing these symptoms, colic can lead to severe stress and, in some cases, postpartum maternal depression.8 With this in mind, it’s best to first educate parents on the prevalence of infant colic and reassure them an end is in sight. Often, infantile colic will resolve within four months.10
When making the assessment it is important to exclude the following conditions:11
- Cows’ Milk Protein Allergy
- Gastro-oesophageal Reflux Disease
- Lactose Intolerance or overload
- Inguinal hernia
- Infection: urinary tract infection, otitis media
- Hydrocephalus
- Non-accidental injury
Breastfed infants should continue with breastfeeding. If a baby is formula-fed, parents should be advised to look out for a nutritionally complete formula that’s specially designed for the dietary management of infantile colic. Always take a comprehensive feeding history as under or over-feeding can affect infants and cause distress. Further history and assessment around crying history, feeding history, sleep and settling and psychosocial areas may be helpful.
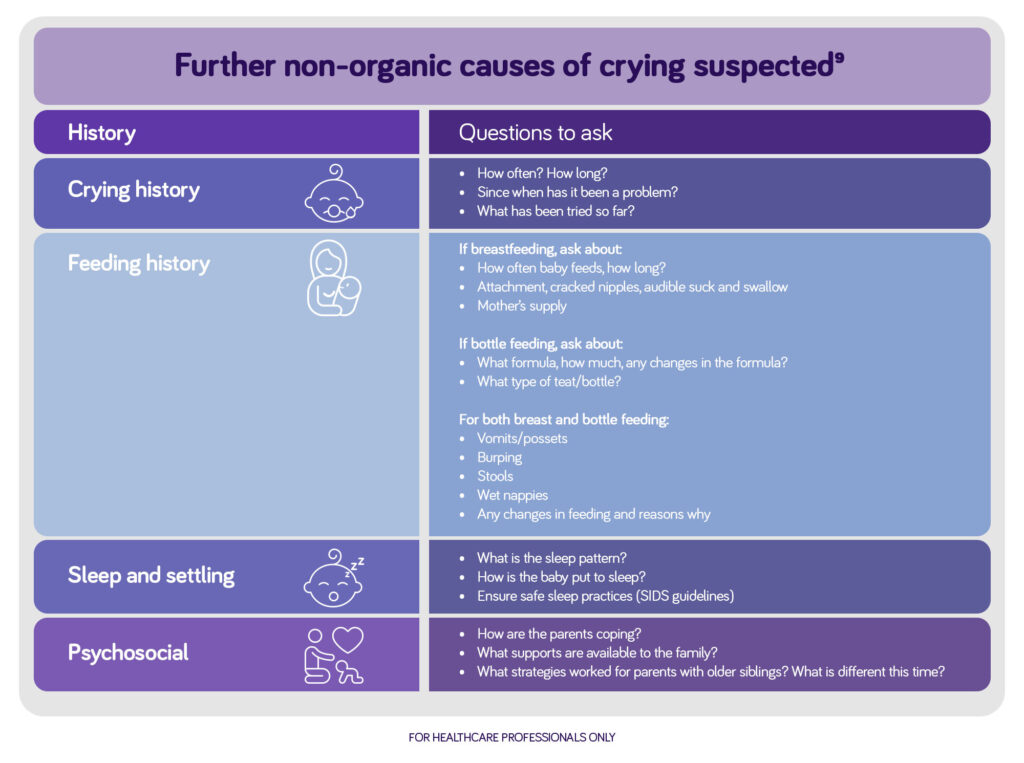
Image: Further non-organic causes of crying suspected9
References
- Vandenplas Y et al. J Pediatr Gastroenterol Nutr 2015;61(5):531-537.
- Quach A. Common neonatal presentations to the primary care physician. Aust J Gen Pract. 2018 Apr;47(4):193-8. PubMed PMID: 29621858. Epub 2018/04/07.
- Benninga MA et al. Gastroenterol 2016; 150(6): 1443-1455.
- Howard CR et al. Breastfeed Med 2006;1:146-55.
- Keefe MR et al. Nurs Res 1996;45:4-9.
- Atkman et al. Arch Dis Child 2006;91:417-9.
- Rauvata et al. Paediatrics 1995;96:43-7.
- Indrio et al. Eur J Pediatr 2015;174:841-2.
- Keefe MR et al. Nurs Res 1996;45:4-9.
- Vandenplas Y et al. Acta Paediatr 2016;105:244-52.
- Sung V. Infantile colic. Aust Prescr. 2018 Aug;41(4):105-10. PubMed PMID: 30116077. PMCID: PMC6091773. Epub 2018/08/18.
Myth Or Fact Around Infantile Colic
Myth: Infantile colic is not a real condition
Fact: Despite no known organic cause, infantile colic can cause distress to infants and families. It has been associated with maternal depression, straining parent-child relationships, shaken baby syndrome, long-term psychological disturbances and is a common cause for early breastfeeding cessation.1,2 Given its prevalence, infantile colic may be associated with an increase in healthcare visits, time off work and trial of unnecessary remedies in an attempt to soothe the distressed infant.1,3,4
Myth: Infants should be the only focus of infantile colic management
Fact: Infantile colic affects more than just the infant. It affects caregivers and the rest of the family as it can have an impact on sleep and ability to work when the infant is sleep-deprived and distressed. Therefore, there are family and financial implications associated with unresolved infantile colic.1,2-4
Myth: Diagnose infantile colic by the rule of threes
Fact: The diagnostic criteria no longer includes Wessel’s rule of threes (where infants had to cry for at least 3 hours per day, for at least 3 days of the week, for the last 3 weeks).7 The latest Rome IV criteria for the diagnosis of infantile colic includes:5
- The infant must be <5 months of age when the symptoms start and stop (crying may peak at 6-8 weeks, improving at 3-4 months).
- Characterised by recurrent and prolonged periods of crying, fussing or irritability that occurs without cause and cannot be prevented or resolved by caregivers (primarily occurs in the late afternoon or evening).
- No evidence of failure to thrive, fever or illness.
Myth: Pharmacotherapy can help resolve the symptoms of infantile colic
Fact: There is little evidence that pharmacotherapy resolves the symptoms of infantile colic.1
FOR HEALTHCARE PROFESSIONAL ONLY
References
- Sung V. Infantile colic. Aust Prescr. 2018 Aug;41(4):105-10. PubMed PMID: 30116077. PMCID: PMC6091773. Epub 2018/08/18.
- Douglas PS, Hiscock H. The unsettled baby: crying out for an integrated, multidisciplinary primary care approach. Med J Aust. 2010 Nov 1;193(9):533-6. PubMed PMID: 21034388. Epub 2010/11/03.
- Akman I, Kuscu K, Ozdemir N, et al. Mothers’ postpartum psychological adjustment and infantile colic. Arch Dis Child. 2006 May;91(5):417-9. PubMed PMID: 16452109. PMCID: PMC2082735. Epub 2006/02/03.
- Howard CR, Lanphear N, Lanphear BP, et al. Parental responses to infant crying and colic: the effect on breastfeeding duration. Breastfeed Med. 2006 Autumn;1(3):146-55. PubMed PMID: 17661591. Epub 2007/07/31.
- Zeevenhooven J, Koppen IJ, Benninga MA. The New Rome IV Criteria for Functional Gastrointestinal Disorders in Infants and Toddlers. Pediatr Gastroenterol Hepatol Nutr. 2017 Mar;20(1):1-13. PubMed PMID: 28401050. PMCID: PMC5385301. Epub 2017/04/13.





