Why Nutrition Matters in Cancer Care
ESPEN recognises the importance of supplementing food with medical nutrition as an integral part of cancer care.² Dietary challenges such as appetite decline and reduced protein intake, and lifestyle choices, such as a plant-based diet, and sensory issues may impact nutritional intake and overall health. ³⁻¹⁰

Appetite decline

Reduced protein intake

Sensory issues

Plant-based lifestyle
Access our Oncology Evidence Booklet and Nutricia Product Range for Cancer Care
- Summaries of the latest clinical evidence to improve patient outcomes
- Explore a range of medical nutrition products to find the most suitable options for your patients.

HCP Detailer

Evidence booklet
Cancer Nutritional Guidelines
Resources

Fortisip Patient Brochure

Malnutrition Screening Tool (MST)

Oral Nutritional Supplement (ONS) Wastage Study
Oncology (UK) Case Study 1
Fortisip Compact Range Evidence Booklet
Oncology (UK) Case Study 2

Bolus Feeding Case Study 1

Bolus Feeding Case Study 2
Learn from Leading Experts
Your Cancer Care, Our Tailored Nutrition
Discover our range of medical nutrition products to find the best option for your patients with cancer.

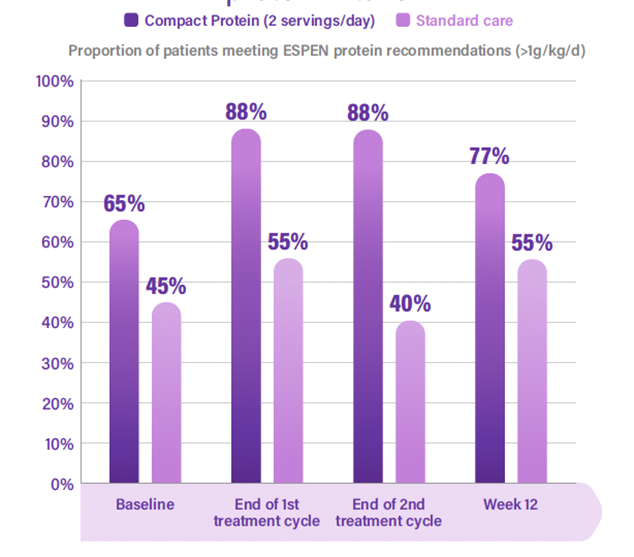
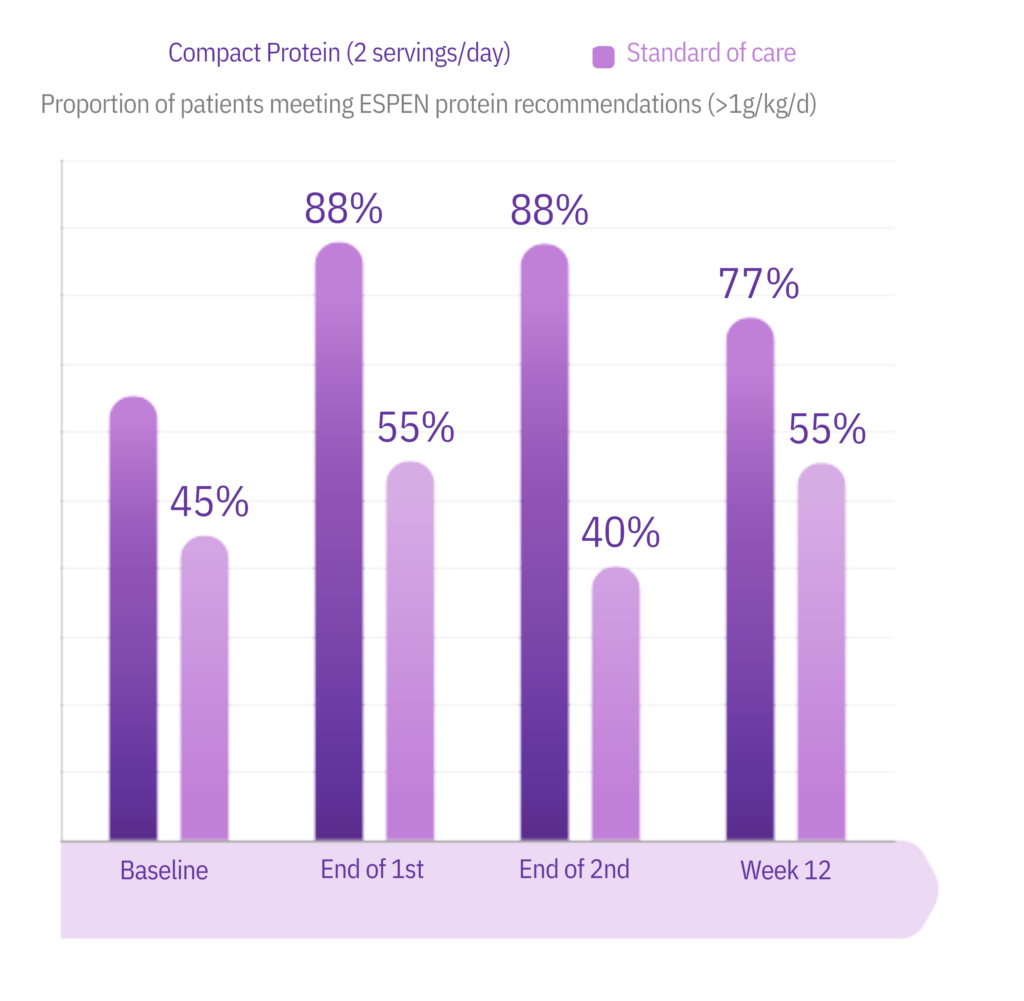
Fortisip Compact Protein, our low volume, high protein formula, enabled patients with cancer to meet ESPEN recommended protein intake.⁶

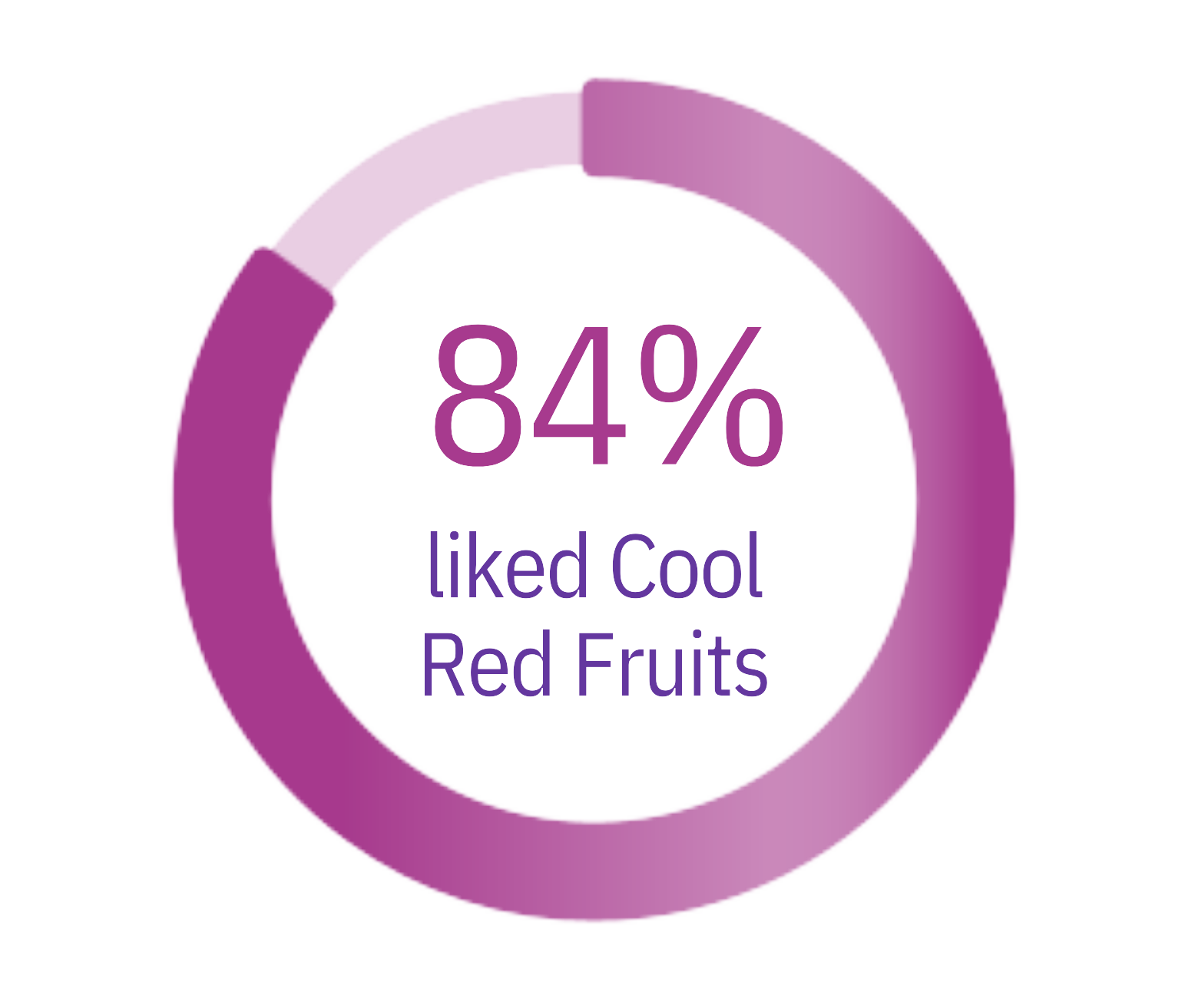
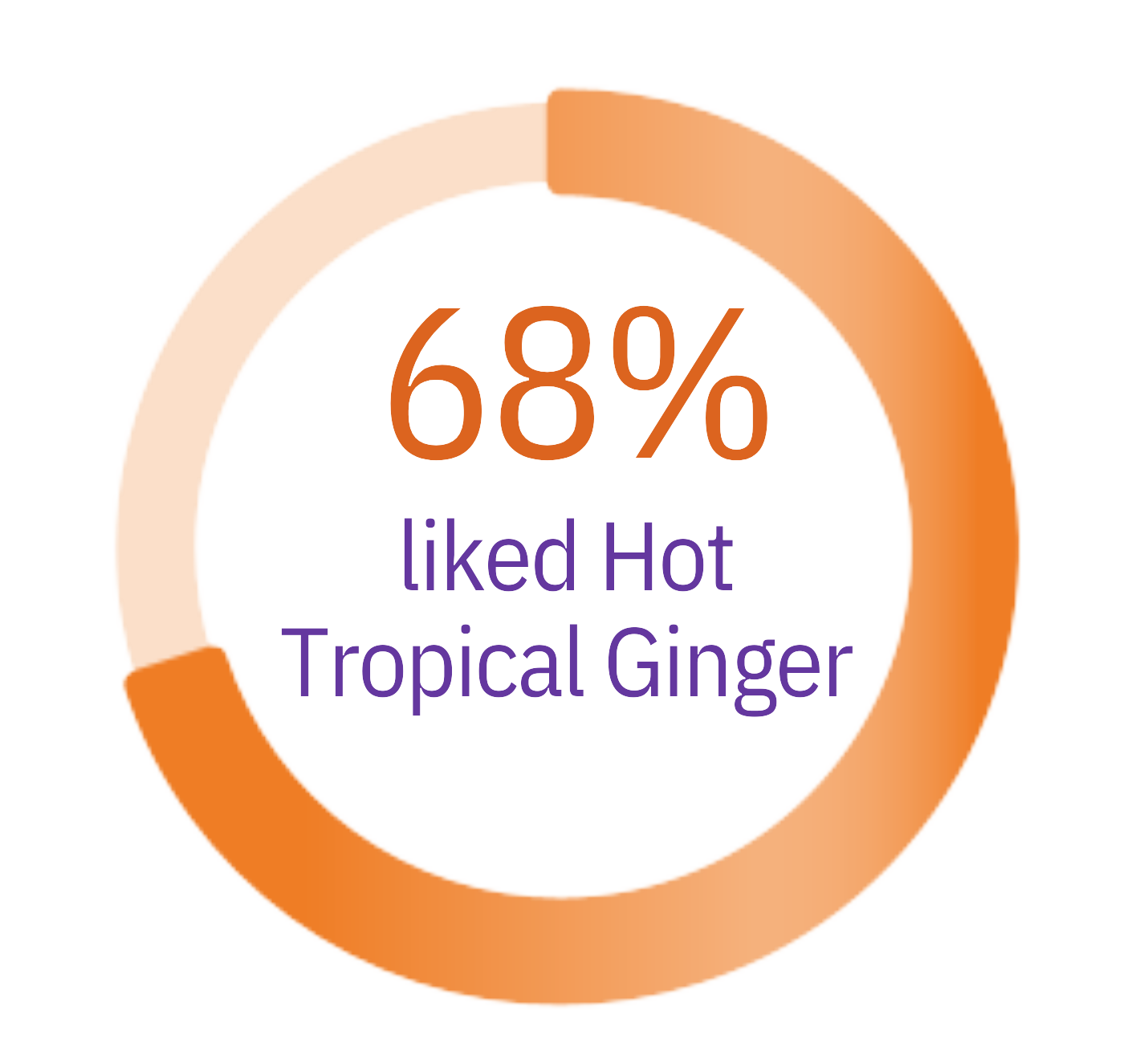
Cancer-related malnutrition and taste alterations
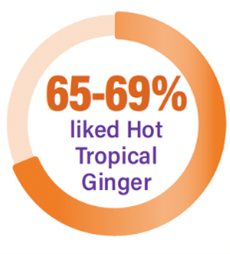
Fortisip Compact Protein Sensations, our compact high protein formula with sensory-adapted flavours, has been validated as ‘liked by patients’ undergoing cancer treatment¹¹ and provides a cool or warm taste sensation.



Cancer-related malnutrition and dairy alternative
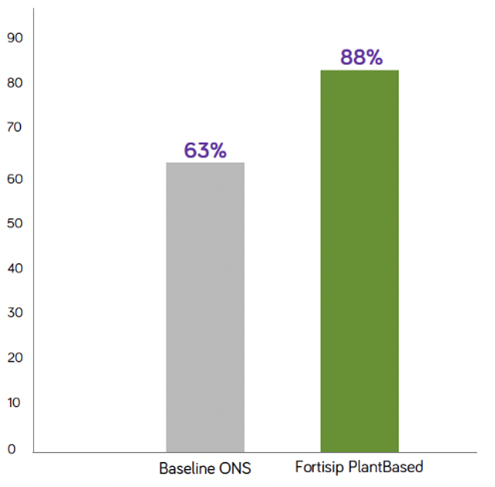
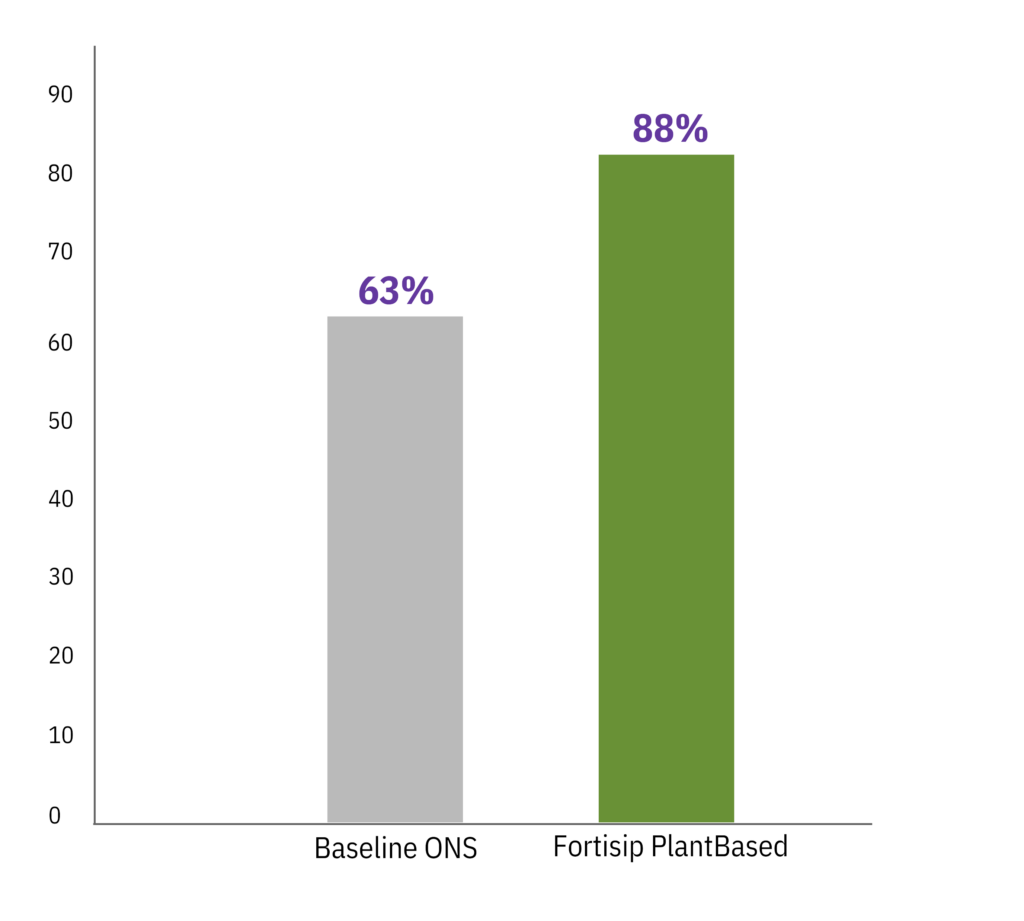
Fortisip PlantBased our unique vegan formula is a high-quality blend of pea and soy protein that achieved greater compliance than baseline~ Prescribed ONS12 and is suitable as a sole Plant-based source of nutrition.#


Help your Patients Access Fortisip®
Explore different ways your patient can purchase Fortisip®, whether through online stores, pharmacies or medical distributors.
Low Volume is Key to Patient Compliance. Small solution = Big difference. (12,13)
Make Fortisip® Compact your first line choice for the intervention of malnutrition. Choose from standard, fibre and high protein options, all in a 125mL format.
Fortisip® Compact in 2 minutes
Fortisip® Product Summary
Supporting Your Patients Beyond Product

Who is The Nutricia Careline?
The Nutricia Careline is a team of trusted dietitians and nutritionists who are here to support and reassure you through your patients and their carers along their oncology journeys. Our caring experts are here to answer all Fortisip questions, big or small.

Nutricia Nursing Service (NNS)
Nutricia’s Nursing Service places high priority on strong clinical governance practices to optimise patient safety and ensure the best possible care for patients during discharge from hospital.
Fortisip products are food for special medical purposes and must be used under medical supervision.
^Compared to healthy adults, whose protein requirements is 0.84 g/kg/day, adults with cancer are recommended to have >1.2g/kg/day and up to 2g/kg/day.
** According to ESPEN guidelines, the additional use of ONS is advised when an enriched diet is not effective in reaching nutritional goals. Medical nutrition is indicated if patients are unable to eat adequately (e.g. less than 50% of the requirement for more than one week or only 50–75% of the requirement for more than two weeks).
~ Prior to commencing the study patients (n=8) were taking a different oral nutritional supplement.
# In accordance with Australia New Zealand Food Standards Code – Standard 2.9.5.
- Caccialanza R, et al. Supp Care in Cancer Jul 2022.
- Muscaritoli M, et al. Oncotarget Advance Publications. Aug 2017;1-13.
- Data on file: IPSOS, Nutrition in Cancer Care survey. 2023.
- Arends J, et al. ESMO Open. 2021;6(3):100092.
- Arends J, et al. Clin Nutr. 2017;36(1):11-48.
- Dingemans AM, et al. Nutrients. 2023;15(24):5030.
- Spotten LE, et al. Ann Oncol. 2017;28(5):969-984
- Brisbois TD, et al. J Pain Symptom Manae. 2011;41:673-83.
- Plant Based Eating. CHOICE 2021. 10. Understanding the New Asian Consumer. PwC, Rabobank and Temasek 2020. Available at: The Asia Food Challenge 2021 (pwc.co.nz) (Accessed September 2023).
- de Haan JJ, et al. Support Care Cancer. 2021;29:5691-9.
- Nutricia UK ACBS trial, data on file 2022.
-
Freeman et al. Aging Clin Exp Res 2011; 23 159
-
Hubbard et al. Clinical nutrition 2012; 31(3): 293-312.