
Malnutrition is common across different groups of older adults and often goes undetected without proper screening. Early identification through routine screening is essential for improving health outcomes.
Together, we can raise awareness and take proactive steps to prevent malnutrition before it starts.
The risk of malnutrition and unintentional weight loss is high across different older patient groups1-3
As little as 5% weight loss is associated with a 50% reduction in activities of daily living4
The greater the weight and muscle loss, the higher the impact on recovery, which can result in4-9:


Malnutrition can have severe consequences for older patients:
- Increased risk of infection2
- 8x increased risk of a harmful fall10
- 4x risk of developing pressure ulcers11
By recognising and addressing malnutrition in your older patients, you can significantly improve their outcomes12-14
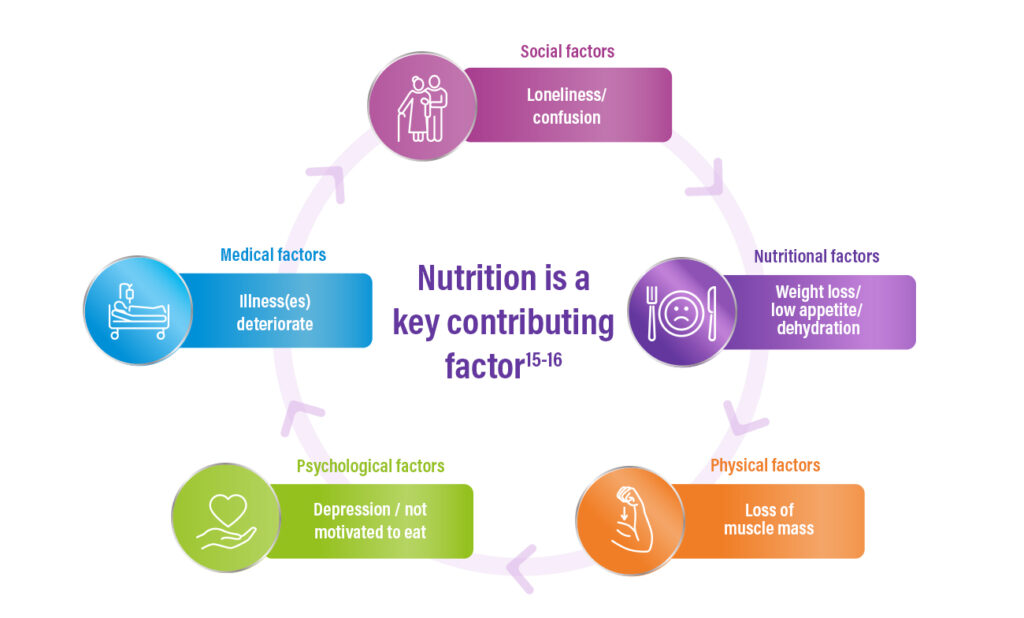
Older patients can find themselves in a vicious spiral of decline leading to frailty & vulnerability.15-16
-
Food intake alone is often insufficient to cover the nutritional needs of older malnourished adults.17,18
- Older adults have up to 2.5 x higher protein requirements17-18
-
1 in 2 are unable to meet these requirements.17-18
ESPEN* Guidelines Recommendation
Nutritional interventions for older people** should be part of a multimodal and multidisciplinary team approach to improve dietary intake, body weight as well as functional and clinical outcomes.19
*ESPEN: The European Society for Clinical Nutrition and Metabolism;
** With chronic conditions when dietary counseling and food fortification are not sufficient
Local2 and International ESPEN Guidelines19 recommend regular screening for all older adults with a recognised assessment tool to identify risk of malnutrition and regular monitoring of those at risk of malnutrition with assessments every 3 months for long-term care residents in a stable condition.
Malnutrition screening can be quick and easy20,21.
Try a validated screening tool such as Mini Nutritional Assessment (MNA)40 and start screening today.
Malnutrition screening is just the first step to appropriate nutritional management

ESPEN* Guidelines19 recommend that ONS offered to an older person with or at risk of malnutrition provide at least 400kcal/day including 30g protein.
Acting quickly with medical nutrition helps improve the quality of life, function and independence of older adults.12,13,22-25
Nutritional intervention with high protein ONS supports malnourished older people to:
- build strength* (1.8kg improvement in hand grip strength)13
- stay out of hospital** (up to 88% fewer hospital readmissions)13,24
- recover faster‡ (around 10 days earlier discharge from rehabilitation)12
- reduce their mortality risk† (around 25% lower risks of mortality at 6 months)25
Nutricia provides a range of nutritional solutions designed to support the diverse needs of older adults who are malnourished or at risk.
Among these, Fortisip Compact Protein with best-in-class evidence, backed by more than 15 studies, over half of which were conducted in older patients with or at risk of malnutrition.22,26-39

ORDER A FREE SAMPLE FOR YOU AND YOUR PATIENTS
Meet our Careline experts


Help your patients access Fortisip
Explore the different ways your patient can purchase Fortisip®, whether through online stores, pharmacies or medical distributors.
For Healthcare professionals only – not to be distributed to general public.
Fortisip® is a food for special medical purposes and must be used under medical supervision.
*A systematic review of patients with malnutrition, majority >65 (83%), receiving an intervention with high protein ONS (>20% energy from protein) vs standard care.
** Malnourished older adults with pneumonia receiving individualised nutritional intervention program vs standard care.
‡ When muscle targeted nutritional interventions are implemented early alongside exercise in hospitalised physical rehabilitation patients vs standard care.
† Malnourished patients with ageing-related vulnerability receiving individualised nutritional care vs standard care ONS: Oral nutritional supplements.
- Sharma Y et al. Journal of nutrition, health and aging. 2017; 21(10): 1210-1215.
- Roberts S, et al. Nutrients. 2021; 13(7):2316.
- O’Shea M-C, et al. Healthcare. 2024; 12(13):1296
- Newman, et al. J Am Geriatr Soc. 2001;49(10):1309-18.
- WHO Global Report on Falls Prevention in Older Age. Available at: 9789241563536_eng.pdf [Accessed November 2024].
- Mühlethaler, et al. Age Ageing. 1995;24(3):193-197.
- Bouziana, et al. J Nutr Metab. 2011;2011:167898.
- Sharkey. Gerontologist. 2002;42(3):373-380.
- Keller, et al. J Gerontol A Biol Sci Med Sci. 2004;59(1):68-74
- Lackoff, et al. J Clin Nurs. 2020;29:429-36.
- Fry, et al. Arch Surg. 2010;145:148-51.
- Rondanelli, et al. J Cachexia Sarcopenia Muscle. 2020;11(6):153.
- Cawood, et al. Ageing Res Rev. 2012;11:278- 96.
- Baumgartner, et al. Nutrition. 2021;89:111279.]
- Clegg, Young. Clin Med. 2011;11(1):72-5.
- Clegg, et al. Lancet. 2013;2;381(9868):752-62.
- Baum, et al. Nutrients. 2016;8;8(6):359.
- Kruizenga, et al. Clin Nutr Open Sci. 2022;41:74-81.
- Volkert, et al. Clin Nutr. 2022;41(4):958-989.
- Vellas, et al. J Nutr Health Aging 2006;10:456–465
- Guigoz et al. J Nutr Health Aging. 2021;25(4):528–583
- Smith, et al. Nutrients. 2020;12(2):517.
- Grönstedt, et al. JAMDA. 2020;21(9):1229-1237.
- Yang, et al. Int J Environ Res Public Health. 2019;16:4758.
- Baumgartner, et al. Nutrition. 2021;89:111279
- Ter Wee, et al. J Nutr Health Aging. 2016;20(9):944-51.
- Grönstedt, et al. JAMDA. 2020;21(9):1229-1237.
- Aldhahir, et al. ERJ Open Res. 2021;7(1):00077-2021. ]
- Brown, et al. J Nutr Health Aging. 2020;24(3):305-11.
- Dingemans, et al. Nutrients. 2023;15(24):5030.
- Frederiksen, et al. Clin Nutr Open Sci. 2022;42:148-159.
- Grupińska, et al. Nutrients. 2021;13(10):3549.
- Leon-Sanz, et al. Front Nutr. 2023;10:1182445
- Obukhova, et al. ESPEN. 23-ABS-1385.
- Pedersen, et al. Trials. 2019;20(1):655.
- Roberts, et al. Abstract LB71-T. Clinical Nutrition ESPEN 58(2023);424-750.
- Torrinhas, et al. Nutr Clin Pract. 2022;37:1152–1161.
- Vikstrom, et al. BMC Geriatrics. 2020;20(1):324.
- Ziętarska, et al. Nutrients. 2017;9(10):1108.
- Nestle Nutrition Institute. https://www.mna-elderly.com/sites/default/files/2021-10/mna-mini-english.pdf [31.07.2025]

